J. Biosci. Public Health. 2025; 1(1)
Background: Myopia, or near-sightedness, is projected to affect nearly five billion people globally by 2050 and is a leading cause of distance visual impairment, posing a major socio-economic burden. Lifestyle factors, particularly increased use of electronic devices, are significant contributors to myopia development in school-going children. Methods: This mixed-method study included 390 school-going children aged 5–12 years diagnosed with myopia. The study was conducted from January 2020 to December 2022. Parents were interviewed using a structured questionnaire, and children's daily screen time was collected through 24-hour recalls. Clinical data were retrieved from diagnostic reports and hospital databases following comprehensive eye examinations, including distance visual acuity, intraocular pressure, and both non-cycloplegic and cycloplegic refraction tests. Results: To observe the effect of screen time and outdoor activities, the study divided the follow-up period into three phases: before, during, and after the COVID-19 pandemic. During lockdowns, children's average screen time increased from 2.1 to 5.6 hours per day, correlating with a significant worsening of refractive errors from -2.4 D to -4.6 D over two years. After the pandemic, as daily screen time reduced to 2.7 hours and outdoor activity increased from 19% to 71%, the progression of myopia slowed notably. Conclusion: Home confinement during COVID-19 markedly accelerated myopia progression in children. Post-pandemic, lifestyle adjustments involving reduced screen time and increased outdoor activities led to stabilization. These findings emphasize the need for balanced digital device use and promoting outdoor exposure to manage and potentially prevent childhood myopia.
Myopia, commonly known as ‘short-sightedness’ or ‘near-sightedness,’ is one of the most prevalent refractive errors globally. This happens when eye length growth and ocular powerare out of balance. The visual images appear blurred because distant objects are concentratedanteriorly to the retinal plane. The refractive error varies from birth to age, although the most significant alterations take place when the eye develops in childhood [1]. Uncorrectedrefractive errors and cataracts are among the leading causes of visual impairment world wide. These conditions carry substantial socioeconomic implications due to their impact on quality of life, productivity, and healthcare costs [2]. Currently, myopia is recognized as a major global public health concern. It is projected that by 2050, approximately 52% of the global population will be affected by myopia-an increase from 27% in 2010 [3]. The prevalence of myopia varies by region, with especially high rates reported in parts of Asia. In countries such as China, Japan, South Korea, Taiwan, and Singapore, myopia affects 80–90% of school-aged children. In European children, the prevalence rises from 7 to 8 years of age, and among teenagers with European blood, the reported prevalence varies from 17 to 36% [4, 5].
The multidimensional causes of emergence and progression of myopia are till now underinvestigation. Genetic, environmental, and lifestyle variables can all be risk factors for young-onset myopia. Emerging evidence highlights the association between myopia and various lifestyle factors, including prolonged screen time, unhealthy dietary habits, reduced outdoor activity, and even mental health issues such as depression. Excessive engagement in near-work activities through digital devices is strongly linked to myopic development and progression in children [6]. As digital devices become more accessible, their use among children has increased rapidly. In 2018, 5% of children aged 5–7 years owned a mobile phone and 42% had access toa tablet. Between 2016 and 2019, average daily screen time among children aged 8 to 12increased by nearly 49 minutes, rising from 4 hours and 18 minutes to over 5 hours per day [7].This rise in screen exposure has raised significant concerns regarding its potential impact on children’s visual health [8]. Several studies have confirmed that prolonged screen use, particularly involving close-range tasks, contributes to the progression of myopia [9, 10].
In response, the American Academy of Optometry has recommended limiting screen time to one hour daily for children aged 2–5 years, and minimizing screen exposure for those over 6years of age [11]. While the exact biological mechanisms are not fully understood, one prevailing theory is that exposure to natural sunlight stimulates dopamine release in the retina, which in turn inhibits axial elongation of the eye–a key factor in the development of myopia[12]. Children with low sunlight exposure and increased near-work activities are found to beat 2.6 times greater risk for developing myopia [13]. Animal studies have also demonstrated that sunlight-induced dopamine release can prevent ocular elongation and myopia progression[14]. Additionally, sunlight boosts Vitamin D synthesis in the skin, which may also influence eye growth and development [15]. Other influencing factors include socio-economic status, sleep patterns, physical activity, and genetic predisposition. Parental history of myopia, poor dietary habits, vitamin D deficiency, and limited exposure to outdoor environments all contribute to an increased risk of myopia among children [16–18]. These factors collectively reduce the exposure to natural light and visual-spatial stimuli, further promoting myopic changes in growing eyes.
In this study, we aimed to explore the impact of lifestyle factors-particularly screen time, outdoor activities, and daily routines-on the progression of myopia in school-aged children. We reviewed the two-year clinical records of 390 children aged 5 to 12 years who were diagnosed with myopia. The study period was divided into three phases: before, during, andafter the COVID-19 pandemic, allowing us to observe the impact of pandemic-related lifestyle changes and providing clinical evidence of the positive effects of a healthy lifestyle-particularlyreduced screen time and increased outdoor physical activities-on the progression of myopia in children. A comprehensive and structured questionnaire was used to gather data directly from the children and their parents, capturing information on visual habits, screen use, dietary patterns, outdoor exposure, and other daily behaviors. By analyzing these variables in relation to myopic progression, this study aims to provide insights that can support targeted public health interventions and early preventive strategies for childhood myopia.
Study Design
This mixed-method study was conducted from January 2020 to December 2022 among the children aged 5 to 12 years who were taking regular follow-up treatment in a specialized eye hospital in Dhaka city. Inclusion criteria encompassed children who were school students, suffering from myopia problems, and willing to participate in this study. Conversely, exclusion criteria included children older than 12 years, those who refused to participate, and those with a history of other types of eye disease or surgical interventions.
Methodology
This study presents a detailed analysis of the vision of 390 children aged 5 to 12 years. Data collection was conducted using a structured questionnaire covering demographic information, daily outdoor activities, engagement in close vision tasks, electronic device usage, mobile phone habits, use of corrective lenses, family history of myopia, and past medical and ocular history. Information regarding the frequency and type of children's daily screen time was collected through parent-reported 24-hour screen time recalls. Follow-up clinical data were obtained directly from diagnostic reports and the hospital database system, with the kind permission of the parents and hospital authorities. A comprehensive diagnostic and prognostic report were prepared for each child based on physical examinations, including measurements of distance visual acuity and intraocular pressure, non-cycloplegic and cycloplegic refraction, etc. An international standard visual chart was used to assess both uncorrected and corrected visual acuity. Refraction was measured under ciliary paralysis using an auto-refractometer (KR-800, Visuref, Tokyo, Japan). The spherical equivalent refraction was calculated as the spherical refractive error plus half of the cylindrical refractive error. Participants with a spherical equivalent refraction of −0.50 diopters
(D) or less in either eye were classified as having myopia. In this study, "before COVID-19" refers to the period up to April 2020, “during COVID-19” covers the period from April 2020 to December 2021 is during the pandemic, and "after the pandemic" denotes the period from January 2022 to December 2022, based on the situation in Bangladesh.
Sample Size calculation
The sample size was calculated using the following equation16:
Here, n = number of samples
z = critical value of the normal distribution
p = expected prevalence estimate
q = (1-p) = expected non-prevalence
d = precision limit or proportion of sampling error
The critical value (z) is included as 1.96 for a 95% confidence level. The precision limit, or
proportion of sampling error (d), is usually considered to be a 5% confidence limit.
Therefore,
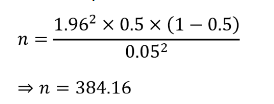
≈ 390 participants were estimated.
Data Analysis Instruments
All data were analyzed using SPSS version 25.0 (SPSS Inc., Chicago, II, USA). Descriptive statistics (percentage, frequency, mean, etc.) and inferential statistics (p-value) were executed
in the study. A chi-square test was used to evaluate the correlations between various kinds of variables. A p-value of <0.05 was set as statistically significant.
Ethical Consideration
All procedures followed the principles of the Helsinki Declaration. Participants were informed about the study's purpose, procedures, and confidentiality, and provided voluntary consent. Written consent was also obtained from the parents or guardians before data collection using a structured questionnaire.
In this study, patient’s information was collected by direct interview of parents using as tructured questionnaire. Table 1 presents the demographic and baseline characteristics of the390 participants. The sample comprised slightly more males (51%, n=199) than females (49%,n=191). Participants were stratified by age: 33.3% (n=130) were 5–7 years old, 35.9% (n=140)were 7–9 years old, 20.2% (n=79) were 9–12 years old, and 21.8% (n=85) were over 12 yearsold. Education levels varied, with the majority in pre-school (54.2%, n=211), followed byprimary (30.0%, n=117) and junior levels (15.8%, n=62). Geographically, 91.8% (n=357)resided inside Dhaka city. Parental income distribution was as follows: 42.6% (n=166) earned>100k monthly, 35.9% (n=140) earned 50–100k, and 21.4% (n=84) earned <50k.Lifestyle factors revealed that only 28.2% (n=110) played outdoor/indoor games, while 71.8%(n=280) did not. Similarly, 18.5% (n=72) read books during leisure time, contrasting with81.5% (n=318) who did not. Regarding screen time, 25.2% (n=98) owned mobile devices,12.5% (n=49) had laptops/computers, and 62.3% (n=243) had no personal electronic devices. A notable proportion (41.5%, n=162) reported a family history of myopia.
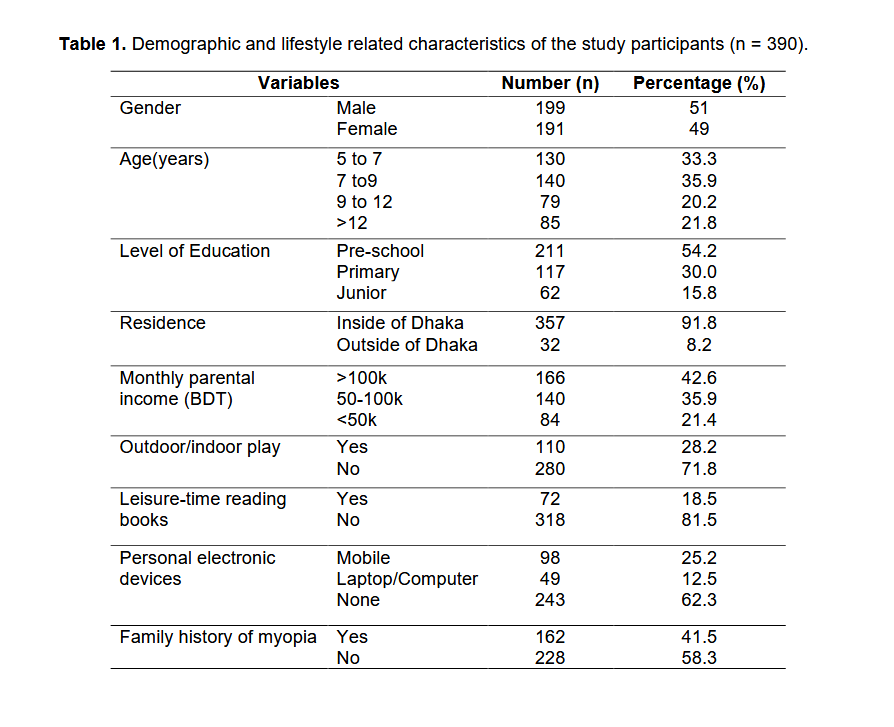
In this study, the association between daily lifestyle behaviors and the rate of myopia progression has been systematically investigated. During the pandemic, the normal lifestyle of school-aged children was disrupted, with the closure of educational institutions and suspension of all outdoor activities like playing, cycling. During this time, students attended classes online from home. Figure 1 illustrates the comparative percentages of children participating in outdoor physical activities before, during, and after the COVID-19 pandemic in Bangladesh. Before the pandemic, 78% of children regularly participated in outdoor activities, whereas only 22% did not. However, during the pandemic, a significant shift was observed: only 18% of children continued outdoor activities, while 82% ceased such activities, coinciding with prolonged school closures and strict public health measures. Following the pandemic, participation in outdoor activities showed recovery, with 72% of children resuming outdoor play, although 28% still refrained from outdoor engagement. Therefore, in next section, spending of time indoor environment by the participants will be investigated.
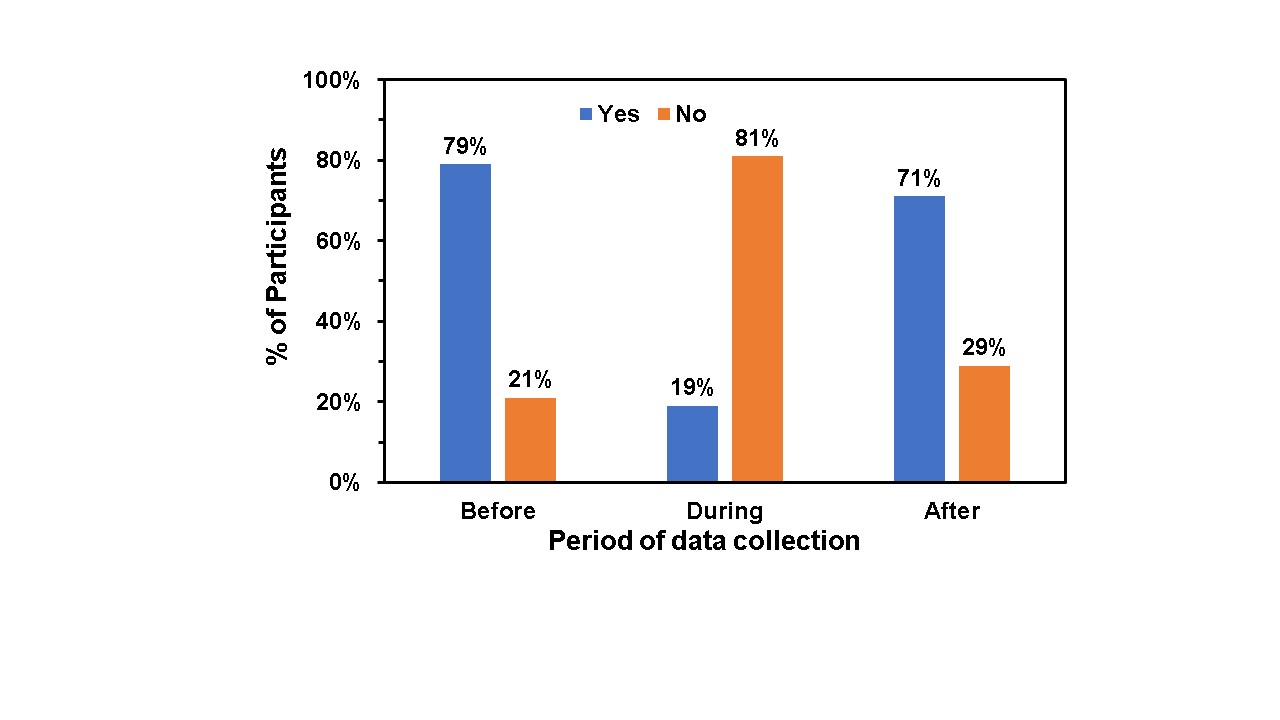
Figure 1. Comparative percentages of children (n = 390) participating in outdoor physical activities (e.g., playing, cycling) before, during, and after the COVID-19 pandemic. In this context, "before COVID-19" refers to the period up to April 2020, "during COVID-19 "covers April 2020 to December 2021, and "after the pandemic" represents the period from January 2022 to December 2022, based on the situation in Bangladesh.
Figure 2 illustrates another factor i.e. indoor lifestyle of children during the pandemic, showing a drastic change in the average daily screen time (±0.5 hours) before, during, and after the COVID-19 pandemic in Bangladesh. Our finding shows that before the pandemic (up to May 2020), the average screen time of children was calculated to be 2.1 ± 0.5 hours/day, including time spent watching TV, using computers, using smartphones, etc. During the pandemic (April 2020–December 2021), screen time surged to 5.6 ± 0.5 hours/day, reflecting a near doubling of usage. Post-pandemic (January–December 2022), screen time decreased slightly to 2.7 ± 0.5 hours/day but remained significantly higher than pre-pandemic levels. These findings highlight a persistent increase in screen exposure among children, likely due to remote learning and habitual shifts. A detailed discussion on the distribution of children's screen time is presented in the subsequent section.
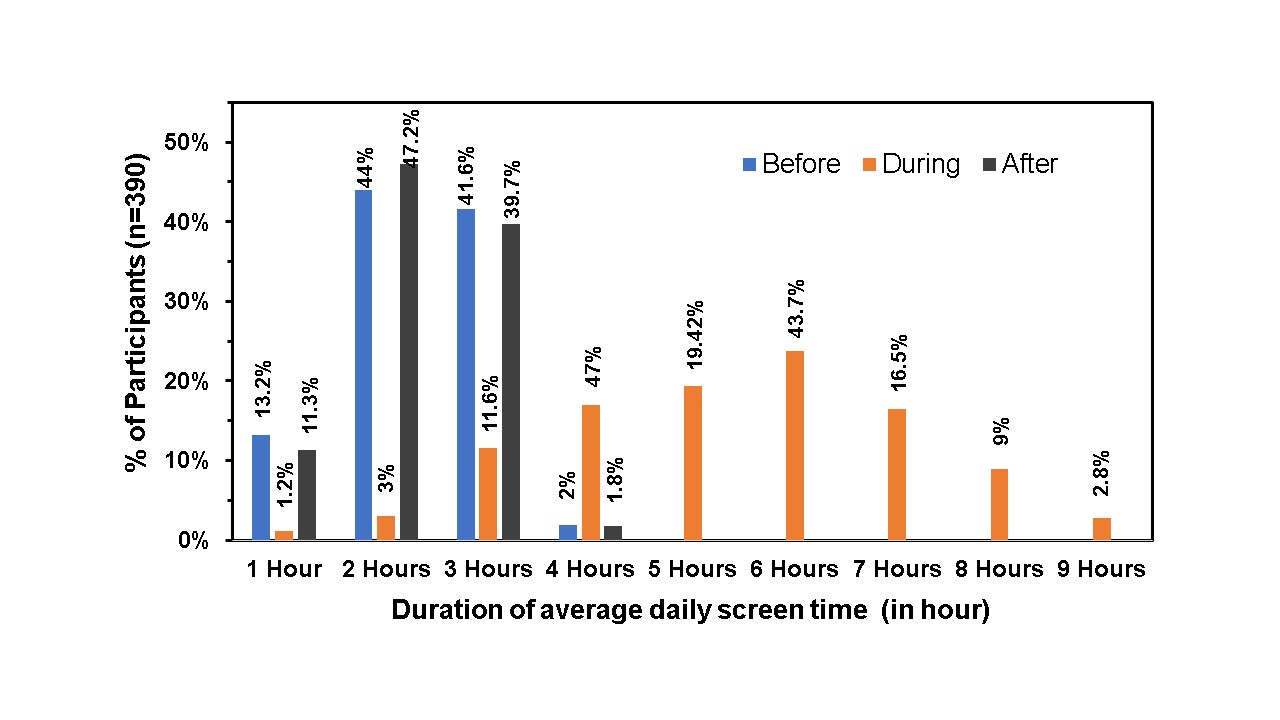
Figure 2. Percentage of children (n = 390) and their comparative average daily screen time(±0.5 hour) before, during, and after the COVID-19 pandemic. Here, "before COVID-19"refers to the period up to May 2020, "during COVID-19" covers April 2020 to December 2021,and "after the pandemic" represents the period from January 2022 to December 2022, based on the situation in Bangladesh.
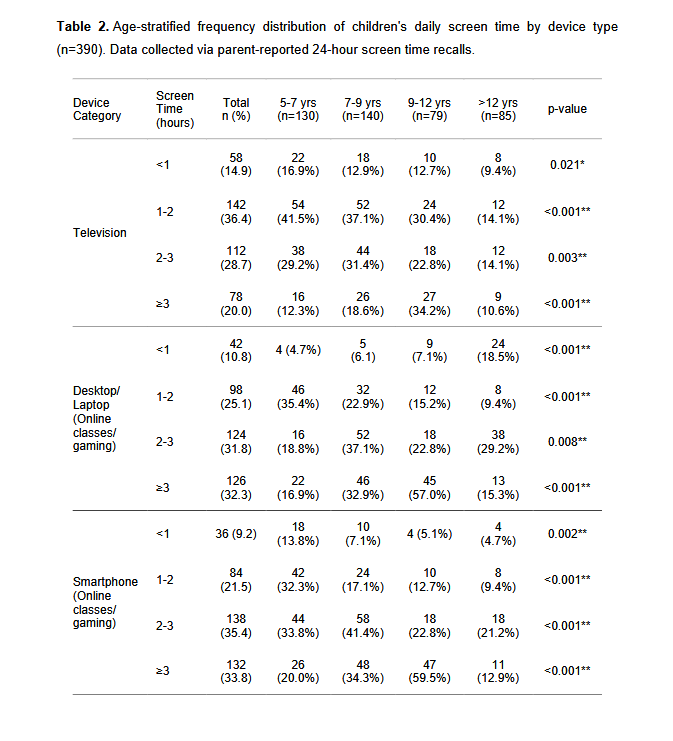
The age-stratified analysis of children's daily screen time revealed significant variations across device types and age groups (Table 3). Television viewing was most prevalent in the 1-2hours/day category (36.4%), with the highest proportion among 5-7-year-olds (41.5%) while digital devices demonstrated more extreme usage. However, desktop/laptop and smartphone usage showed markedly different patterns, with 57.0% of 9-12-year-olds using desktops/laptops for ≥3 hours/day (p<0.001) and 59.5% of the same age group using smartphones for ≥3 hours/day (p<0.001). Moreover, 32.3% of 5-7-year-olds used smartphones1-2 hours daily. Notably, screen time increased with age for all devices, peaking in the 9-12-year-old group before declining slightly in the >12-year-old group. Desktop/laptop use was 4-times higher than TV in 9-12-year-olds for ≥3 hours. Accordingly, the subsequent sectionpresents the impact of altered screen time on myopia progression, based on clinical datacollected during the study period.
Figures 3, illustrates the longitudinal progression of myopia in school-going children by tracking the average lens powers of both eyes from January 2020 to December 2022. The results are showing at the beginning of COVID-19 (Jan 2020), the average lens powers of both eyes of the children were from -2.2 to -2.7 (±0.82). The follow-up results at every 6 month sinterval data clearly presenting during the COVID-19 lockdown, from June 2020 to June 2021,power of lens was significantly increasing with average power of left lens -3.7 (±0.63) and right eye -4.5 (±0.85). As stated earlier, after June 2022, with the easing of lockdown restrictions, daily screen time decreased to 2.7 hours (±0.5), and outdoor physical activities increased by 71%. Consequently, the results show that the progression of myopia began to slowdown in both eyes.
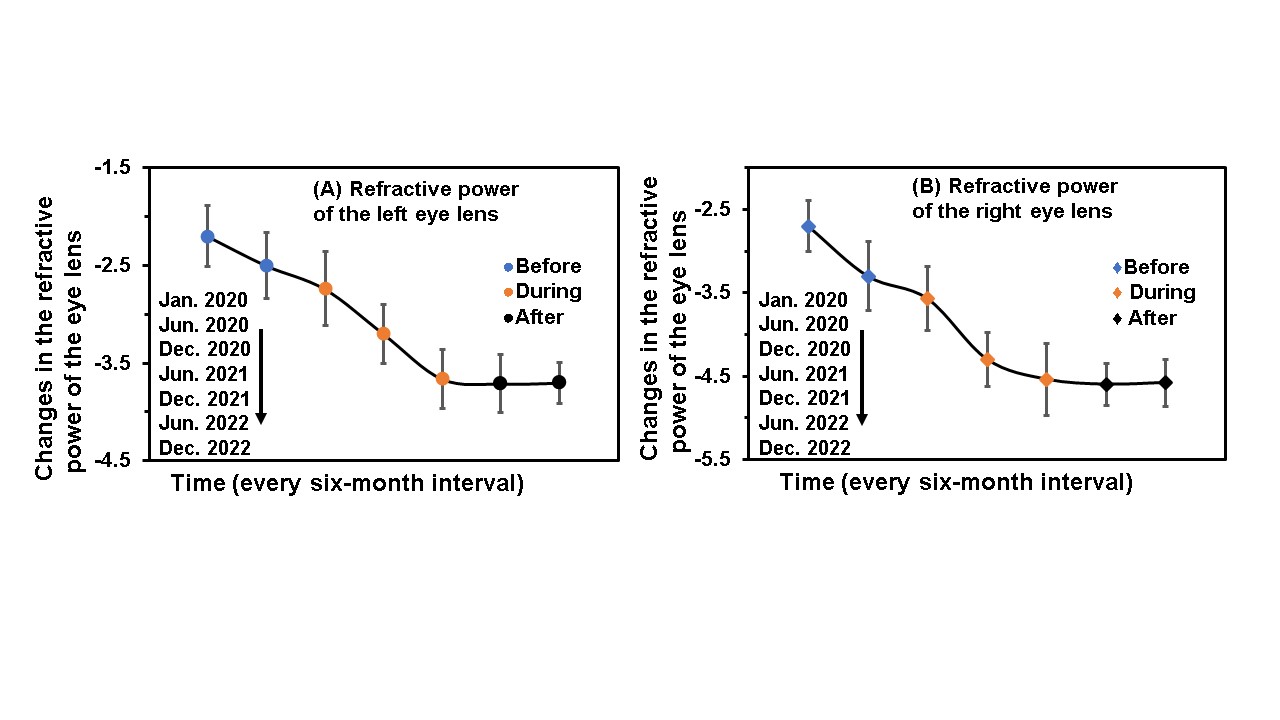
Figure 3. Estimated average changes in lens power among participants, recorded at six-month intervals (±1 month) from January 2020 to December 2022. A total of 203 participants (52%of the initial 390) consistently continued follow-up throughout the study period. In this study,data from January and June 2020 represent the “before COVID-19" period, "during COVID-19" covers December 2020 to December 2021, and the "post-pandemic" period refers fromJune 2022 to December 2022, based on the COVID-19 situation in Bangladesh.
As established in previous studies [20, 21], myopia is influenced by genetic factors,environmental conditions, and gene–environment interactions. Although socio-economicdisparities and family history may also contribute to the risk of myopia, this study specificallyfocused on the impact of prolonged screen time and reduced outdoor activities on theprogression of myopia among school-going children in Bangladesh. The dramatic rise in screen time during the pandemic correlates with global trends of increased digital device use for education and leisure [22]. Prolonged screen exposure is a known risk factor for myopia progression due to near-work strain and reduced outdoor activity [23]. Consistent with globaltrends, an increase in screen time and a decrease in physical activity were observed amongchildren in this region. Given that outdoor activities have a protective effect against myopia progression, the decline in such activities may have exacerbated the prevalence of myopia in school-aged children [24]. Similar trends were observed in the post-pandemic period, likely due to sustained screen dependency and altered daily routines.
During the lockdown period, time sharply increased screen time leading to increased accommodative demand and reduced blinking rate-factors implicated in axial elongation and myopia development [25]. The data demonstrate a clear association between increased screen time during the COVID-19 pandemic and accelerated myopia progression in children. These findings align with previous studies which report similar trends [26]. Although screen time declined after COVID-19, it did not revert to baseline, suggesting enduring behavioral changes. This sustained elevation may exacerbate myopia incidence, as studies associate >2 hours/day of screen time with faster myopic shifts [27]. Interestingly, after the normalization of pandemic restrictions, a statistically slow down progression in both eye’s refractive error was observed, alongside a substantial reduction in daily screen time. This suggests that lifestyle modifications, such as increasing outdoor time and reducing near work, may halt myopia progression in some cases [28].Chromaticity signals may be important for normal eye growth, which may partly explain why outdoor activity has a protective effect against myopia. Both ambient lights emitting diode(LED) illumination and digital screens emit a high proportion of wavelengths at the blue end of the visible spectrum, and these wavelengths have been associated with axial growth. For example, tree shrews tended to become more myopic when raised in blue light, while exposure to red LEDs inhibited axial eye growth [29]. Therefore, it is necessary to support ongoing efforts to limit electronics screen exposure and promote balanced visual habits among children. Schools, healthcare providers, and parents should work collaboratively to integrate vision-friendly practices, such as the 20-20-20 rule (every 20 minutes, look at something 20 feet away for 20 seconds) and regular eye checkups, especially in populations with high baseline screen use [30].
The findings of this study indicate a notable increase in the incidence of myopia among school- going children in Dhaka during the COVID-19 pandemic, correlating with a significant reduction in outdoor activities and a marked increase in near-work tasks i.e. prolong electronics screen-time. As children transitioned back to normalcy post-pandemic, improvements were observed across various parameters, including reduced screen time, resumption of physical outdoor activities, healthier life styles, and better sleeping routines. Nonetheless, the overall improvement or stabilization trend provides encouraging evidence that modifiable lifestyle factors can play a critical role in mitigating myopia development in children. These findings emphasize the importance of maintaining balanced visual habits, encouraging outdoor play, and minimizing unnecessary screen exposure in school-going children to support ocular health and potentially slow the progression of myopia.
We extend our heartfelt gratitude to all those who contributed to the successful completion of this research project. We are immensely grateful to the Bangladesh Eye Hospital authority, who allowed us to interview their patient`s parents, for the collection of data and follow-up reports.
This research was conducted with self-funding. Therefore, any kind of financial support was not received for this study.
The authors declare no conflict of interest. All aspects of this research were conducted impartially and independently. No financial or personal relationships with other people or organizations have influenced this work.
This study did not involve any experiments on human participants or animals; therefore, formal written informed consent was not required. However, oral consent was obtained from all participants prior to data collection. Moreover, ethical approval was obtained from the Institutional Review Board of Primeasia University (PAU) (Ref: PAU/IEAC/22/12) prior to data collection, ensuring the privacy and confidentiality of participants were upheld throughout the study.

This work is licensed under a
Creative Commons Attribution 4.0 International License
.
You are free to share and adapt this material for any purpose, even commercially, as long as you give appropriate credit.