J. Biosci. Public Health. 2026; 2(1)
The implementation of occupational health and safety (OHS) in hospitals plays an essential role in protecting both medical and non-medical staff from the risks of injury, infection, and work-related stress. Although OHS regulations are in place, their implementation often remains suboptimal due to various interrelated factors. This review aims to identify and analyze the determinants that influence the implementation of OHS in hospitals. This study is a scoping review conducted using the framework of Arksey and O’Malley (2005), which includes five stages: identifying the research question, searching for relevant studies, selecting studies, extracting data, and summarizing the findings. Literature searches were performed across five databases (ProQuest, PubMed, ScienceDirect, EBSCO, and Wiley) with the inclusion criteria of quantitative observational studies published in English between 2010 and 2025. Out of 17927 articles, eleven (11) met the inclusion criteria and were analyzed. The synthesis showed that the determinants influencing the implementation of OHS in hospitals include the level of knowledge, motivation, compliance, education, years of service, training and supervision, work stress, competence, actions, policies, standard operating procedures, leadership, human resources, and law enforcement. Demographic factors such as age, gender, and education were also found to be associated with OHS implementation levels. The implementation of OHS in hospitals is influenced by a combination of individual, organizational, and structural factors. Strengthening training, leadership, compliance with institutional policies, and developing a multidimensional intervention model are crucial for the successful implementation of effective OHS practices for healthcare workers.
Occupational Health and Safety (OHS) is a critical component in ensuring the protection and well-being of medical and non-medical personnel in hospital environments [1]. Hospitals are among the most complex workplaces, characterized by high exposure to biological hazards, chemical agents, physical injuries, ergonomic risks, and psychosocial stressors [2-4]. These conditions require effective OHS implementation to prevent work-related accidents, occupational diseases, and declines in worker performance. International evidence consistently shows that strong OHS systems contribute to reduced injury rates, improved employee health, enhanced productivity, and better organizational outcomes in healthcare settings. Despite the existence of regulatory frameworks and guidelines for OHS, many hospitals particularly in low- and middle-income countries continue to experience suboptimal implementation, indicating the presence of various systemic and individual barriers [5].
Although numerous studies have examined factors influencing OHS in hospitals, most existing research tends to focus on isolated determinants such as knowledge, stress, leadership, or standard operating procedures [6, 7]. These studies often analyze one or two factors at a time, resulting in fragmented understanding of how determinants interact within the broader OHS system. Furthermore, many studies are context-specific and concentrated in certain regions, limiting their generalizability and failing to provide a comprehensive picture of the interrelated determinants that jointly influence OHS implementation. Existing reviews, including integrative and descriptive literature reviews, primarily emphasize OHS culture or safety climate but do not holistically map determinants across individual, organizational, and structural domains [8]. Consequently, the literature still lacks a broad synthesis that integrates diverse factors and presents a more holistic, system-level view of OHS implementation [9, 10].
Another gap identified in previous studies is the absence of clear justification regarding why certain determinants exert influence and how their interactions shape OHS performance in hospitals [11]. Some studies also do not explicitly assess the methodological strengths or weaknesses of included evidence, making it difficult to determine the reliability of their conclusions. Additionally, inconsistencies in the reported findings with some studies identifying knowledge or training as significant while others highlight organizational or policy-level determinants underscore the need for a comprehensive mapping effort that synthesizes heterogeneous evidence [12, 13].
Therefore, a scoping review is warranted to systematically map, categorize, and synthesize the broad range of determinants influencing OHS implementation in hospitals. Unlike traditional systematic reviews, scoping reviews are designed to explore complex topics with diverse study designs, summarize existing knowledge, and identify research gaps that require future investigation. This review specifically responds to the limitations of previous literature by (i) compiling studies from multiple settings and methodological backgrounds, (ii) analyzing interrelated determinants rather than isolated variables, and (iii) providing a comprehensive overview of individual, organizational, and structural factors. Through this approach, the present scoping review aims to offer more holistic and integrated insights that can support policymakers, hospital administrators, and researchers in designing targeted interventions to strengthen OHS implementation in hospital environments. The aim of this study is to identify and analyze various determinants that influence the implementation of occupational health and safety (OHS) in hospitals.
This scoping review systematically synthesizes research evidence on the determinants influencing the implementation of occupational health and safety (OHS) in hospitals, despite variations in research objectives and methodologies. The framework used in this review follows the [14] methodological approach, which provides a structured process for conducting scoping studies.
2.1. Identifying the Research Question
The research question in this scoping review was developed using the PCC framework (Population, Concept, and Context) to examine the determinants of the implementation of occupational health and safety (OHS) in hospitals.
Here, Population (P): Hospital workers; Concept (C): Determinants or factors influencing the implementation of occupational health and safety (OHS), and Context (C): Hospitals, including both public and private institutions.
This PCC format helps to focus the review on hospital workers as the study population and to explore various factors affecting the success of OHS implementation within the hospital setting. Based on this framework, the guiding research question of this scoping review is:
“What are the main determinants influencing the implementation of occupational health and safety (OHS) in hospitals?”
2.2. Identifying Relevant Studies and Search Terms
After defining the research question, this review followed the Joanna Briggs Institute (JBI) search strategy [15] to identify determinants of OHS implementation in hospitals. The next step involved identifying relevant studies by determining the keywords and phrases used in the search process.
In total, five electronic databases were used for this scoping review: ProQuest, PubMed, ScienceDirect, EBSCO, and Wiley. The initial search involved extracting titles, abstracts, and content to identify appropriate keywords. The keywords used for each database are presented in Table 1. The Garuda and Google Scholar databases were excluded from the search because they are categorized by some researchers as sources of grey literature.
Keyword extraction was performed by reviewing titles, abstracts, and full texts to identify relevant and alternative terms suitable for each database context. The inclusion and exclusion criteria were based on the Population–Concept–Context (PCC) framework proposed by [16]. The population included healthcare workers. This review focused on quantitative observational studies published in English between 2010 and 2025, with open-access full articles. English was chosen as it is the primary language of global scientific communication, and most international publications are written in English.
Table 1. Keywords used in the search.
| Database | Keywords | Total Articles | Remaining After Screening | Access Date |
| Google scholar | ("occupational health and safety" OR "workplace safety" OR "occupational safety") AND ("implementation" OR "factors" OR "determinants") AND ("hospitals" OR "healthcare institutions") AND ("challenges" OR "barriers" OR "effectiveness" OR "outcomes") | 17600 | 310 | 27-11-2025 |
| ProQuest | ("occupational health and safety" OR "workplace safety" OR "occupational safety") AND ("implementation" OR "factors" OR "determinants") AND ("hospitals" OR "healthcare institutions") AND ("challenges" OR "barriers" OR "effectiveness" OR "outcomes") | 2,211 | 89 | 24-Nov-24 |
| PubMed | ("occupational health and safety" OR "workplace safety" OR "occupational safety") AND ("implementation" OR "factors" OR "determinants") AND ("hospitals" OR "healthcare institutions") AND ("challenges" OR "barriers" OR "effectiveness" OR "outcomes") | 79 | 2 | 24-Nov-24 |
| ScienceDirect | ("occupational health and safety" OR "workplace safety" OR "occupational safety") AND ("implementation" OR "factors" OR "determinants") AND ("hospitals" OR "healthcare institutions") | 12,395 | 241 | 26-Nov-24 |
| EBSCO | ("occupational health and safety" OR "workplace safety" OR "occupational safety") AND ("implementation" OR "factors" OR "determinants") AND ("hospitals" OR "healthcare institutions") | 248 | 45 | 26-Nov-24 |
| Wiley | ("occupational health and safety" OR "workplace safety" OR "occupational safety") AND ("implementation" OR "factors" OR "determinants") AND ("hospitals" OR "healthcare institutions") AND ("challenges" OR "barriers" OR "effectiveness" OR "outcomes") | 3,262 | 116 | 26-Nov-24 |
2.3. Study Selection and Data Extraction
Figure 1 presents the process and results of article screening using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram, along with the extraction criteria applied after the initial search based on inclusion and exclusion parameters.
In summary, a total of 17927 relevant articles were retrieved from the seven databases. After removing duplicates and screening according to the inclusion and exclusion criteria, 648 articles remained. The next step involved screening the articles based on their titles and abstracts, resulting in 648 articles for full-text review. Following the full-text screening, 648 articles met the eligibility criteria, and based on their relevance to the research question, 11 articles were finally included for analysis. The eligible articles were then presented in a data extraction table, organized, categorized, and summarized for further synthesis.
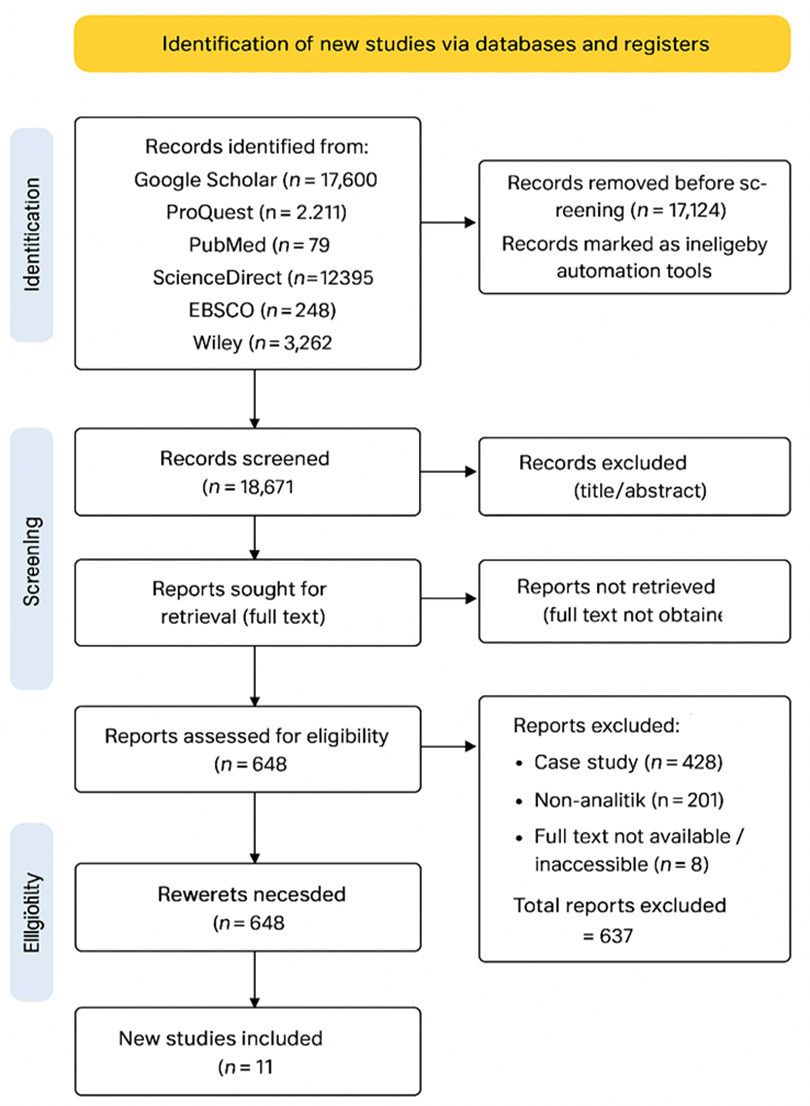
Figure 1. PRISMA flow diagram illustrating the article screening process and final selection.
2.4. Data Mapping
In line with JBI recommendations, this scoping review also conducted a methodological quality appraisal of all included studies. While quality appraisal is optional in scoping reviews, incorporating it provides a clearer understanding of the robustness of current evidence. The JBI Critical Appraisal Checklist for Analytical Cross-Sectional Studies was used to assess key methodological domains. The results of this appraisal were not used to exclude studies but were integrated into the interpretation of findings to enhance the credibility and contextualization of the review outcomes.
Data were independently extracted manually based on the JBI (Joanna Briggs Institute) Manual for data extraction, which includes the characteristics of each study and the research methods described and presented in tabular form. The factors influencing the implementation of occupational health and safety (OHS) programs in hospitals were identified, and the variables measured are listed in Table 2.
Table 2. Characteristics of included studies on determinants of OHS implementation in hospitals.
| Reference | Study objective | Population and sample size | Study design | Key results | Main determinants / conclusions |
| Yamin et al., Indonesia [17] | To examine the association between nurses’ knowledge, motivation, and compliance and OHS implementation | 76 nurses, Mega Buana Palopo Hospital | Quantitative cross-sectional | Good OHS implementation in 55.3% of nurses; knowledge (p=0.012), motivation (p=0.034), and compliance (p=0.016) significantly associated | Knowledge, motivation, and compliance significantly influence OHS implementation |
| Tukatman, Indonesia [18] | To identify determinants of OHS program implementation among nurses | 100 nurses from four hospital units | Cross-sectional | Education level, years of service, training, and supervision significantly associated with OHS; training strongest predictor (OR = 10.043) | Education, experience, training, and supervision are key OHS determinants |
| Wiratna & Chei, Indonesia [19] | To analyze effects of workload, job stress, and competence on SMK3RS implementation | 442 staff; 100 nurses sampled | Cross-sectional | Workload, stress, and competence explained 19.05% of SMK3RS implementation variance | Job stress and competence directly affect OHS management system implementation |
| Deseva et al., Indonesia [20] | To identify organizational factors influencing OHS implementation | 915 staff; 100 sampled | Analytical cross-sectional | Actions, policies, SOPs, and leadership significantly influenced OHS; policy most dominant factor | Organizational policies, SOPs, and leadership drive OHS implementation |
| Ulfa et al., Indonesia [21] | To assess determinants of SMK3 implementation | 118 staff, Lirboyo General Hospital | Cross-sectional | Human resource quality (p=0.003) and law enforcement (p<0.001) significant; supervision not significant | Human resources and law enforcement are critical to OHS system performance |
| Ngoga et al., Kenya [22] | To examine factors influencing OHS measures among healthcare workers | 146 healthcare workers | Mixed-methods cross-sectional | Training, leadership support, and demographics significantly predicted OHS compliance | Training, leadership, and governance structures strengthen OHS implementation |
| Ma et al., China [23] | To assess incidence and risk factors of occupational exposure among pediatric HCWs | 1,932 HCWs from 43 hospitals | Cross-sectional survey | Occupational exposure prevalence 93%; profession, education, work environment, and self-protection awareness significant | Individual, organizational, and relational factors influence exposure risk |
| Cheng et al., Taiwan [24] | To identify factors associated with needlestick and sharps injuries among dentists | About 1,300 dentists nationwide | Cross-sectional survey | 23% reported NSSI; recapping, workload, experience, and lack of training increased risk | Unsafe behaviors, workload, and inadequate training increase injury risk |
| Wu et al., China [25] | To examine determinants of workplace violence against physicians | Clinical physicians (multi-hospital sample) | Cross-sectional | Poor communication, heavy workload, low security, and job stress increased violence risk | Organizational support and work environment influence workplace violence |
| Dewi & Wardani, Indonesia [26] | To assess association between OHSMS components and work accidents | 152 nurses | Analytical cross-sectional | Leadership, policies, procedures, and training significantly reduced accidents | Strong OHSMS implementation lowers work-related accident rates |
| Nowrouzi et al., Canada [27] | To explore facilitators and barriers to OHS implementation | SMEs, healthcare-related settings | Descriptive cross-sectional | External inspections and management commitment improved safety practices | Regulatory oversight and leadership facilitate OHS implementation |
| Ullah et al., Pakistan [28] | To evaluate effect of work safety on organizational social sustainability | Public hospital staff | Cross-sectional | Supervisory safety behavior and coworker attitudes positively predicted sustainability | Safety climate and supervisory behavior enhance organizational sustainability |
2.5. Organization, summary, and reporting of results
The results of this review were reported through descriptive analysis and a narrative summary of the findings, presented using both text and tabulation. The reporting process followed the methodological framework and stages of the [14] scoping review approach.
Table 3. Quality appraisal of included studies using JBI checklist.
| Study (Reference) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | Total | Quality |
| Yamin et al. [17] | Yes | Yes | No | Partial | No | No | No | Yes | 4/8 | Moderate Quality |
| Tukatman et al. [18] | Yes | Yes | Yes | Partial | Partial | Yes | Partial | Yes | 6.5/8 | Moderate–High Quality |
| Alfian Yoga Wiratna et al. [19] | Yes | Partial | Partial | Yes | Yes | Partial | Partial | Yes | 6/8 | Moderate Quality |
| FriscaGemmi Deseva et al. [20] | Yes | Yes | Yes | Partial | Partial | Yes | Partial | Yes | 6.5/8 | Moderate–High Quality |
| Ulfa et al. [21] | Yes | Partial | Partial | Partial | Yes | Yes | Partial | Yes | 4/8 | Moderate Quality |
| Ma et al. [23] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 8/8 | High Quality |
| Chen et al. [24] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 8/8 | High Quality |
| Wu et al. [25] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 8/8 | High Quality |
| Dewi & Wardani [26] | Yes | Yes | Partial | Yes | Partial | No | Yes | Yes | 6/8 | Moderate–High Quality |
| Nowrouzi et al. [27] | Yes | Yes | Partial | Partial | Yes | Yes | Partial | Yes | 5/8 | Moderate Quality |
| Ulla Z. et al. [28] | Yes | Yes | Yes | Yes | Partial | Partial | Yes | Yes | 6/8 | Moderate–High Quality |
*JBI quality appraisal criteria in Table 3 as follows:
1.Inclusion criteria clearly defined.
2.Study subjects and setting described in detail.
3.Exposure measured in a valid and reliable way.
4.Objective, standard criteria used for outcome measurement.
5.Confounding factors identified.
6.Strategies to deal with confounding stated.
7.Outcomes measured in a valid and reliable way.
8.Appropriate statistical analysis used.
Scoring system:
“Yes” = 1 point; “Partial” = 0.5 point; “No” = 0 points.
Total scores ranged from 0 to 8. Studies were categorized as High Quality (≥7 points), Moderate–High Quality (5–6.5 points), or Moderate Quality (<5 points).
The methodological quality of the eleven articles included studies was assessed using the JBI Critical Appraisal Checklist for Analytical Cross-Sectional Studies. As presented in Table 3, the majority of the studies demonstrated strong methodological rigor, with four articles categorized as high quality and two articles classified as moderate-to-high quality. Most studies clearly defined inclusion criteria, described the study population and setting in sufficient detail, and employed valid and reliable measurements for both exposure variables and OHS-related outcomes.
Across the included studies, confounding factors were generally identified and addressed, although variation was observed in strategies used to manage these confounders. The representativeness of samples and adequacy of sample size were also evaluated positively in most studies. However, a few studies showed minor methodological limitations, particularly in the areas of sample representativeness and clarity of statistical analysis, resulting in slightly lower quality ratings.
Overall, the quality appraisal indicates that the evidence base included in this scoping review is methodologically sound and provides reliable insights into the determinants of OHS implementation in hospitals. The integration of quality appraisal findings into the narrative synthesis enhances the interpretability and credibility of the review's conclusions.
3.1. Study Characteristics
The studies analyzed in the table generally employed a cross-sectional research design, which is widely used to identify factors associated with the implementation of OHS in hospitals. All studies used a quantitative approach with structured questionnaires, either developed by the researchers or based on nationally and internationally validated instruments. Sample sizes varied considerably, ranging from small studies involving 76 nurses to large-scale national surveys with more than 1,900 healthcare workers. Most studies were conducted in Indonesia, reflecting a strong emphasis on the implementation of the Hospital Occupational Health and Safety Management System (SMK3RS). However, studies from China, Taiwan, Kenya, Pakistan, and Canada broaden the analytical perspective by presenting OHS practices in various healthcare systems and organizational structures.
The primary aims of these studies were to identify determinants of OHS implementation or occupational hazard exposure, focusing particularly on individual, organizational, and systemic factors. Some studies explored relationships between variables such as knowledge, motivation, years of service, workload, and supervision, while others examined risk factors related to needlestick injuries, workplace violence, or occupational exposure among healthcare workers. Methodologically, the analytical techniques varied from simple chi-square tests and logistic regression to more complex procedures such as Structural Equation Modeling (SEM), reflecting differences in analytical depth across studies. Overall, these varied study characteristics provide a comprehensive understanding of OHS implementation across healthcare settings in both developing and developed countries.
.
3.2. Determinants of OHS Implementation in Hospitals
(i). Individual Determinants
Individual-level determinants such as knowledge, motivation, experience, competency, stress, and risky behaviors significantly influence OHS implementation. Yamin et al. [17] demonstrated that nurses’ knowledge and motivation were strongly associated with adherence to OHS practices. Tukatman [18] emphasized that years of service, training exposure, and educational background significantly enhanced compliance. Wiratna and Chei [19] reported that job stress and employee competence directly influenced the implementation of SMK3RS. Risky behaviors, especially related to sharps handling, were highlighted by Cheng et al. [24], who found that recapping, improper disposal, and inconsistent use of protective equipment increased the risk of needlestick and sharps injuries. Similarly, Ma et al. [23] noted that lower self-protection awareness and dissatisfaction with work conditions elevated occupational exposure risks among pediatric healthcare workers. These findings underscore that individual skills, attitudes, and psychological conditions play key roles in shaping safe practices within hospitals.
(ii). Organizational Determinants
Organizational factors emerged as the strongest predictors of OHS implementation across most studies. Deseva et al. [20] found that policies, standard operating procedures (SOPs), leadership, and organizational actions significantly influenced OHS implementation, with policy identified as the most dominant factor. Tukatman [18] reported that training profiles were the most influential determinant (OR = 10.043), while supervision and education level also played key roles. Dewi and Wardani [26] highlighted that strong leadership, effective procedures, and structured policies significantly reduced workplace accidents among nurses. Similarly, Ulfa et al. emphasized the role of human resource quality and legal enforcement [21], both of which significantly affected the implementation of SMK3 in hospitals. Organizational safety culture also played a crucial role; stressed that inadequate security, heavy workloads, and low organizational support increased workplace violence risk [25]. These studies collectively show that strong leadership, updated policies, regular training, supportive supervision, and adequate staffing are essential organizational drivers of OHS implementation.
(iii). Systemic and Environmental Determinants
Systemic-level determinants such as external regulations, professional relationships, and national OHS policies also shape hospital safety performance. Ma et al. [23] reported that a harmonious doctor–patient relationship reduced occupational exposure risks, while overcrowded environments and strained communication heightened hazards. Ngoga et al. [22] emphasized the importance of county-level governance in Kenya, recommending the establishment of OHS committees and policy enforcement mechanisms at the hospital and government levels. Nowrouzi et al. [27] found that external safety inspections significantly contributed to safer work environments in Canadian SMEs, demonstrating the critical role of external oversight and compliance monitoring. Another systemic perspective has been highlighted the influence of organizational safety climate on social sustainability; their findings showed that job safety, supervisory safety behavior, and coworker attitudes strongly predicted positive sustainability outcomes [28], while management safety practices were perceived as weak due to poor implementation and oversight. These findings illustrate that broader sociocultural, regulatory, and governmental frameworks substantially influence OHS behaviors and outcomes in hospitals.
3.3. Multilevel Determinants of OHS Implementation Based on the Socio-Ecological Model
The multilevel analysis of determinants influencing Occupational Health and Safety (OHS) implementation in hospitals, based on the Socio-Ecological Model (SEM), shows that OHS practices are shaped by interacting factors at the individual, interpersonal, organizational, community, and policy/system levels. At the individual level, determinants highlighted in several reports include knowledge, motivation, competency, work experience, job stress, risk perception, and self-protection awareness [17-19. Inadequate knowledge, low motivation, high stress, or unsafe behaviors such as needle recapping noted by Cheng et al. [24] increase the likelihood of occupational accidents and weaken compliance with OHS procedures. At the interpersonal level, supervisory guidance, peer support, and professional relationships significantly shape safety behaviors. Tukatman [18] found that nursing supervision positively influenced OHS practices, while Ulla Z. et al. [28] demonstrated that supervisory safety roles and coworker safety attitudes strengthened adherence to safety protocols. Positive doctor–patient interactions, as noted by Ma et al. [23], also reduce risks such as violence or occupational exposure.
At the organizational level, most studies identify institutional structures and management systems as the strongest determinants of OHS implementation. Some research emphasized the critical role of leadership, internal policies, SOPs, and safety procedures, with policy emerging as one of the most dominant predictors of OHS compliance [20, 26]. Additionally, training, human resource quality, legal enforcement, and organizational capacity revealed as key contributors to successful OHS programs [18, 21]. Environmental and work condition factors such as hospital security, workload, and staffing identified by Wu et al. [25] further influence workers’ ability to implement safety practices. At the community level, broader hospital–patient relationships, safety culture in the healthcare environment, and the external professional community shape safety norms. The findings of Ngoga et al. [22] underscore the role of community awareness and institutional culture in reinforcing occupational safety, especially in resource-limited settings.
Finally, at the policy/system level, external regulations, monitoring mechanisms, and governmental support exert significant impacts on OHS implementation. Nowrouzi et al. [27] demonstrated that external safety inspections greatly improved safety performance in healthcare organizations. Similarly, the role of county-level governance highlighted by Ngoga et al. [22] shows that system-level policies, regulatory oversight, and safety governance structures are essential for sustaining safety practices. Evidence from another study indicates that systemic gaps such as outdated safety policies or weak management involvement can hinder organizational social sustainability and undermine safety programs [28]. Taken together, the SEM-based synthesis shows that OHS implementation in hospitals is not determined by a single factor, but rather by a dynamic interaction of determinants across multiple ecological levels, with organizational and policy-level influences serving as the strongest drivers of safety performance (Figure 2).
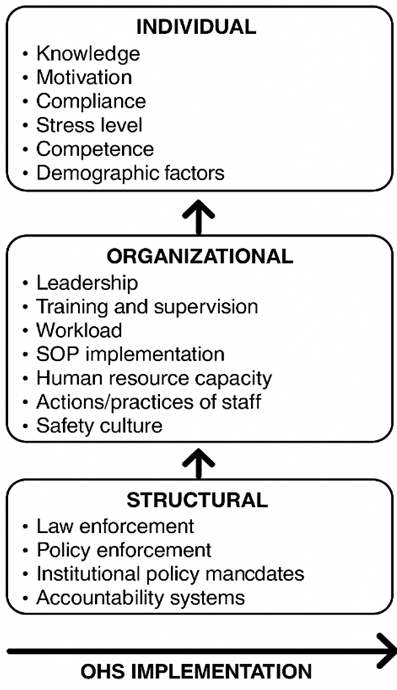
Figure 2. Conceptual model based on the Socio-Ecological Model (SEM).
The findings of this scoping review indicate that determinants of OHS implementation in hospitals operate across multiple levels and vary significantly by context. Several studies consistently identified individual-level factors such as knowledge, motivation, and compliance as important contributors to OHS adherence. However, other studies reported no significant association between knowledge or attitudes and actual OHS practice, highlighting contradictions that suggest individual determinants may not be sufficient on their own to drive safe behavior. Similar inconsistencies have been reported in previous safety research, which shows that worker behavior is strongly influenced by broader organizational and contextual conditions rather than individual factors alone [29].
Variability was also observed in organizational-level determinants. Leadership, supervision, and SOP enforcement were frequently identified as strong predictors of effective OHS implementation, aligning with Safety Climate Theory, where employees’ perception of management commitment and communication practices shape their safety behaviors [30]. Nevertheless, some studies found that organizational interventions such as training yielded limited improvements, particularly in settings with high workloads or insufficient staffing. Such discrepancies align with the idea that safety climate is not only determined by formal systems but also by the consistency and credibility of leadership behavior [31].
Integrating theoretical perspectives helps to explain these variations. According to the High Reliability Organization (HRO) Theory, organizations that excel in safety maintain a strong “preoccupation with failure,” organizational learning capacity, and resilience traits that differentiate high-performing hospitals even under resource constraints [32]. The findings of this review suggest that only hospitals with strong HRO characteristics such as vigilant supervision, responsive leadership, and consistent SOP enforcement demonstrate robust OHS implementation regardless of individual worker attributes. This explanation is supported by evidence showing that high-resilience hospitals sustain better safety outcomes even in complex environments [33].
The findings carry significant implications for low- and middle-income countries (LMICs) compared with high-income countries. Because most studies included in this review were conducted in LMICs, structural determinants such as law enforcement, regulatory compliance, resource availability, and institutional accountability emerged as more influential compared to organizational culture alone. Weak enforcement of safety policies and chronic resource limitations in LMICs can undermine OHS implementation even when workers possess adequate knowledge or motivation. In contrast, evidence from high-income settings suggests that organizational-level factors (e.g., communication quality, safety climate, and reliability systems) are typically the main drivers of safety outcomes [34]. These differences underscore the need for LMICs to prioritize structural reforms such as stronger regulatory oversight, adequate budget allocation, and stricter accountability with microcredential-based health education before higher-order interventions can be fully effective [35].
Overall, the synthesis of findings reinforces that OHS implementation is shaped by multilevel and interacting determinants, consistent with the Socio-Ecological Model (SEM). Individual skills and motivation must be supported by organizational leadership and structural policies to produce meaningful improvements. This integrated interpretation highlights the need for multi-level strategies combining individual training, organizational culture strengthening, and systemic policy enforcement to advance OHS implementation, especially in resource-limited hospital environments.
This scoping review demonstrates that the implementation of occupational health and safety (OHS) in hospitals is shaped by a complex interaction of determinants operating at individual, organizational, and system levels. Individual factors that affect compliance to OHS processes include knowledge, motivation, competence, work experience, and stress, yet they are insufficient. The most reliable and significant factors influencing successful OHS implementation were found to be organizational determinants, specifically leadership commitment, training and supervision, enforcement of standard operating procedures, human resource capability, and institutional regulation. Safety performance is further enhanced at the system level by supportive governance structures, external monitoring, and regulatory enforcement. Regardless of individual worker characteristics, the overall analysis shows that hospitals with supportive safety systems and strong organizational leadership achieve better OHS outcomes. On the other hand, even when healthcare professionals are motivated and have sufficient knowledge, OHS implementation is hampered by lax monitoring, insufficient resources, and poor policy enforcement. These results emphasize how crucial it is to approach OHS from a multilevel, systems-based perspective that is in line with the Socio-Ecological Model. Overall, improving OHS implementation in hospital settings requires integrated interventions that combine workforce training with strong leadership, clear policies, effective supervision, and robust regulatory support. Future research should focus on longitudinal and intervention-based studies for developing sustainable OHS systems, particularly in resource-limited healthcare environments.
The authors gratefully acknowledge Department of Nursing, Faculty of Medicine, Halu Oleo University and all colleagues for their kind support and cooperation. Approximately 10% of the text and reference formatting involved AI-assisted support, in accordance with the journal’s policy.
There is no funding source to carry out this study.
The authors declare no conflicts of interest.
This study did not involve human participants or animals; therefore, formal informed consent and Institutional Review Board approval were not required. All figures were created by the author. Author is solely responsible for any kind of misinformation.

This work is licensed under a
Creative Commons Attribution 4.0 International License
.
You are free to share and adapt this material for any purpose, even commercially, as long as you give appropriate credit.